Treating Fibromyalgia with Acupuncture
Published on March 5, 2015 by Dr. Caitlin Gordon
 Fibromyalgia (FM) means “pain of the muscle fiber,” and the most characteristic symptom is a high level of pain in muscle tissue. It wasn’t until 1987 that the American Medical Association (AMA) recognized it as a “distinct condition that is responsible for significant disability (Marcus, 1).”
Fibromyalgia (FM) means “pain of the muscle fiber,” and the most characteristic symptom is a high level of pain in muscle tissue. It wasn’t until 1987 that the American Medical Association (AMA) recognized it as a “distinct condition that is responsible for significant disability (Marcus, 1).”
The typical sufferer of fibromyalgia is: female, over 30, and has some combination of the following symptoms:
- widespread musculoskeletal pain,
- stiffness,
- fatigue,
- weakness, and
- disordered, non-restorative sleep.
It is common for patients to have digestive issues and symptoms that are exacerbated by cold weather, stress, and overexertion (Pfaffenberger, 2). Symptoms are often worse in the mornings. Women are more affected than men in a ratio of 8:1 (Pfaffenberger, 1). In women between the ages of 70 and 79, the prevalence is 7.4%. The disorder can be found in most countries, ethnic groups and all climates.
Fibromyalgia and the Western Medical System
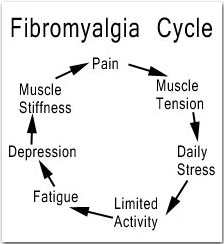
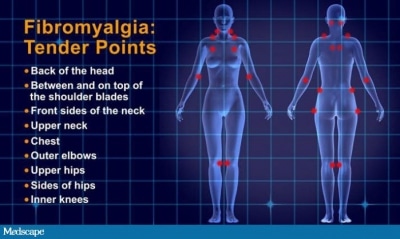 Western medicine finds this difficult to diagnose, as laboratory tests will not show evidence of inflammation and there is no evidence of muscle damage causing pain. A combination of a history of widespread pain for at least 3 months as well as a positive pain response on 11 of 18 tender point sites designated by the American College of Rheumatology is used to diagnose the condition. There is very high consistency among FM sufferers with tenderness at these point locations (Wang, 2). Western medicine currently treats FM with pain medication and/or anti-depressants. There are very few theories as to why the disease develops. FM may be triggered by medical illness, surgery, trauma or emotional stress (Pfaffenberger, 1). The following disorders are commonly associated with FM: irritable bowel syndrome, irritable bladder, headaches (including migraine headaches), dysmenorrhea, premenstrual syndrome, restless leg syndrome, and TM (Pfaffenberger, 1).
Western medicine finds this difficult to diagnose, as laboratory tests will not show evidence of inflammation and there is no evidence of muscle damage causing pain. A combination of a history of widespread pain for at least 3 months as well as a positive pain response on 11 of 18 tender point sites designated by the American College of Rheumatology is used to diagnose the condition. There is very high consistency among FM sufferers with tenderness at these point locations (Wang, 2). Western medicine currently treats FM with pain medication and/or anti-depressants. There are very few theories as to why the disease develops. FM may be triggered by medical illness, surgery, trauma or emotional stress (Pfaffenberger, 1). The following disorders are commonly associated with FM: irritable bowel syndrome, irritable bladder, headaches (including migraine headaches), dysmenorrhea, premenstrual syndrome, restless leg syndrome, and TM (Pfaffenberger, 1).
The symptoms of FM may be transient in nature and may vary significantly in severity.
Fibromyalgia and Traditional Chinese Medicine
Chinese medicine can be helpful in treating fibromyalgia, but realistic expectations must be outlined. Patients often have been through years of tests and attempts at treatment in both the western medical system and sometimes alternative medicine and may have minimal patience and financial resources remaining. Acute phases of symptoms can be managed, but it is important to understand that acupuncture will be a long-term process since this is a chronic condition. Patients need to be willing to commit to possibly many months of treatment to achieve a significant reduction in symptoms. Even then, flare-ups are to be expected. The goal is to reduce the intensity and frequency and duration of these episodes.
Recent Research on Acupuncture & Fibromyalgia
Studies on FM are grouped into those that looked to treat a specific symptom associated with the condition, such as insomnia, or Reynaud’s and those that looked to reduce pain. Because FM is characterized by a set of common symptoms, it is difficult to review research on the condition as a whole. Acupuncture has been shown to be effective for pain, depression, insomnia, and other associated symptoms in a large number of clinic trials. Here I include three summaries of studies on FM.
- In the first, 10 random controlled studies were chosen among 25 and over 1500 participants due to low risk of bias. Acupuncture was shown to reduce the number of tender points and pain scores compared with conventional medicines. It showed no significant difference in effect on pain between acupuncture and sham acupuncture (Cao, 397). A combination of acupuncture and cupping showed greater pain reduction and improved depression scores than conventional medications (Cao, 397). The study concluded that “TCM therapies appear to be effective for treating FM. However, further large, rigorously designed trials are warranted because of insufficient methodological rigor in the included trials (Cao, 397).”
- The second trial examined 50 FM patients in a randomized controlled trial. The study found a significant improvement in symptoms of fatigue and anxiety in the patients who received acupuncture compared with the control group. (Mayo). David Martin, a Mayo clinic anesthesiologist said, “the results of the study convince me there is something more than the placebo effect to acupuncture…it affirms a lot of clinical impressions that this complementary medical technique is helpful for patients (Mayo).” There were minimal side effects and no adverse effects in the Acupuncture.
- The third study was a look at nine randomized trials of nearly 400 participants with a low risk of selection bias (Deare, 1). Three studies used Electro-stimulation acupuncture (EA) and the remainder used manual acupuncture. One used trigger points and the remainder used TCM formula acupuncture. The study states that there is “low to moderate-level evidence that compared with no treatment and standard therapy, acupuncture improves pain and stiffness in people with fibromyalgia (Mayo).” The study concluded that EA was better at reducing pain and stiffness as well as improvement of sleep and fatigue than manual acupuncture (Mayo).
Each of the studies I read through mentioned that exercise therapy was shown to be moderately effective in reducing FM symptoms compared to all other interventions. This appears to be the most consistently effective therapy. From a TCM perspective, this probably breaks up stagnation in the body by helping move qi, blood, and drain phlegm as well as improving the patient’s mood which relieves some of the emotional energy drain on the Liver and Spleen.
Diagnosis and Differentiation
(This section is geared towards TCM practitioners)
 Most acupuncturists will treat FM in their career as one in five fibromyalgia sufferers use acupuncture treatment within two years of diagnosis (Deare, 1). There are a vast number of ways to go about treating FM and it depends entirely on the individual patient. Because FM is not one or two organs out of harmony, but a set of symptoms relating to many organ systems it is difficult to generalize as to which diagnosis and differentiation theoretically should be used and followed. For the sake of discussion, from my research of expert opinions I have included 4 common broad patterns that may underlie FM.
Most acupuncturists will treat FM in their career as one in five fibromyalgia sufferers use acupuncture treatment within two years of diagnosis (Deare, 1). There are a vast number of ways to go about treating FM and it depends entirely on the individual patient. Because FM is not one or two organs out of harmony, but a set of symptoms relating to many organ systems it is difficult to generalize as to which diagnosis and differentiation theoretically should be used and followed. For the sake of discussion, from my research of expert opinions I have included 4 common broad patterns that may underlie FM.
1. Liver Qi Stagnation
Patients tend to display this pattern at an early stage of FM syndrome. It often follows a stressful life event, which knots up the qi and stagnates the liver—the organ associated with anger and repressed emotions (Maciocia). This pattern may also arise later in the progression of the disease when many other treatment efforts have failed and patients are “disillusioned and embittered by life and feel unable to make positive changes (Pfaffenberger, 3).” Symptoms of Liver Qi Stagnation include migraines, variable and poorly localized pain, throbbing pain, anxiety, muscle stiffness in shoulders and neck, irritable bowel syndrome and waking frequently during the night. The tongue may be swollen and red along the edges or look dusky. The Pulse will be wiry or tight, especially in the Liver position (Maciocia).
Qi stagnation slows down circulation, which may lead to heat or blood stagnation. This will intensify the pain the patient experiences and may lead to insomnia or worsening headaches. Liver often begins to overact on the spleen in these cases, which leads to the next common pattern of Spleen qi and blood deficiency. The stagnation and depressed spleen function will create damp in the body, further obstructing the flow of qi and blood.
Treatment for these patients should be aimed at soothing liver qi, moving blood, and if necessary, clearing heat. Good points are LV 3, LI 4, GB 34, Ren 12, UB 18, UB 19, yintang, and anmian (Cheng).
2. Qi and Blood Deficiency
This is usually Spleen Qi and blood deficiency. The Liver overacts on the spleen impeding its transporting and transforming function (Maciocia). The clear yang does not rise to the head, which can lead to symptoms of forgetfulness, “brain fog”, trouble focusing and dull headaches. The patient often experiences chronic fatigue, muscle weakness, and numbness, dream disturbed sleep, depression and doesn’t wake feeling rested (Maciocia). The tongue is pale with thin white fur, and usually puffy with teeth marks or a quiver. The pulse will be thready weak and deep. The lack of restful sleep may be the most important perpetuating factor for FM patients. Because they cannot repair and restore blood during the yin time of night, they feel fatigued which only depresses their ability to cope with pain (Maciocia). As this pattern progresses, damp will accumulate in the channels. These patients often report that their pain is worse with cold and damp weather and that there is heavy quality to it. Digestive issues will escalate or make their first appearance. Often patients will alternate between constipation and diarrhea or have pain after eating. If left untreated, damp will turn into phlegm which is more difficult to treat and will obstruct the channels further (Maciocia).
The treatment plan should be to tonify the spleen, drain damp, and help build blood by improving the spleen function. However, one should be careful not to overtonify in a patient with any pathogenic factors or who is already very stagnant. This will make symptoms worse and drive a pathogen in deeper (Maciocia). Good points to use are ST 36, SP 3, SP 9, LI 4, KD 3, HT 6, UB 17, UB 20, SP 10 (Cheng). Moxa is also indicated to help tonify and increase red blood cell production.
3. Qi stagnation and blood stasis
Patients with qi stagnation and blood stasis experience burning or gnawing pain along with numbness and tingling. The tongue will be dusky, purple, and have swollen subs. These patients have often been experiencing FM symptoms for several years. Many are on painkillers, which further stress the liver and increases stagnation (Marcus, 4). The liver cannot nourish the tendons or sinews and the blood cannot circulate properly. Exercise is important for these patients as it will help move qi and break up the blood stasis. According to acupuncturist Alon Marcus, “When Blood stasis is significant the patient may develop abdominal reactions at the left lower quadrant, visible darkened blood vessels, skin discoloration (especially lips), choppy or slippery/wiry pulse, and a hard area or point (fibrous tissue) within the muscle, often at the motor points (usually at midpoint of muscle), and fixed pain that is worse at night or by inactivity (Marcus, 4).”
Treatment should focus on moving qi, breaking up stagnation and moving blood to alleviate pain. Good points are DU 20, LV 3, LI 4, UB 17, UB 18, SP 10, PC 6, LI 10 with strong stimulation and Tuina on painful channels (Cheng). Marcus suggests using microsystems as well. He notes that because a sensation of swelling and distention (without actual swelling) is common in FM patients, the following points can help: SP 4, LU 7, UB 11, ST 37, ST 39 and SP 21 for total body pain (Marcus, 3).
4. Kidney deficiency (yin, yang, qi or essence)
In long term illness or pain patterns, the vital substances of the body are exhausted and Kidneys inevitably become depleted. They are the source of yin and yang and have a close relationship with the Heart, Liver, and Spleen (Maciocia). Kidney Yang will fail first which leads to blood stasis and increased pain. The fire that the Heart and San Jiao use to circulate fluid and blood come from the Kidneys and without their proper functioning, all FM symptoms become more severe. Symptoms include impotence, lack of libido, sore low back and knees, restless leg syndrome, hot flashes, night sweats, menstrual disorders and irritable bladder (Maciocia). The tongue will be dry, peeled, and have cracks. It might also be very pale or purple. The pulse will be thin and weak and deep in the kidney position in particular. At this point in the disease progression, the patient may be experiencing all of the patterns discussed above and will likely be at a pain level that makes daily functioning difficult.
Treatment should focus on tonifying all qi, yin, and yang. Herbs are especially important for helping the kidneys function better. Good points are Ren 3, 4, 6, KD 3, 6, 7, Sp 6, UB 23, 31, and GB 39 (Cheng).
Case Studies
Because FM can be complex, case studies help illuminate how patterns are diagnosed and treatment relieves symptoms. I read through many case studies to see if I could find some common threads, which would help reveal the most effective path of treatment. Often FM diagnoses are preceded by a very stressful life event like a death in the family or a divorce or a serious (usually infectious) illness. Also, childbirth late in life was a commonality. All of these etiologies are associated with deficiency of qi and blood. Emotionally stressful life events deplete both the Heart and Spleen and stagnate the Liver. These three organs are most responsible for maintaining a healthy balance of qi and blood (Maciocia). Chronic illness and childbirth later in life are very taxing for the kidneys and always leads to blood deficiency. While some experts believe FM can be caused by a latent pathogen, most case studies were consistent with a chronic history of deficiency-particularly the Heart, Spleen, and Kidneys. TCM theory supports a diagnosis of stagnation or excess with symptoms like insomnia and muscle pain in some cases; however, the chronic nature of FM symptoms and the digestive disturbances and lethargy often experienced are common TCM deficiency symptoms.
Case studies I read also support the view that dietary changes are important for relieving symptoms like fatigue, digestive upset, and mind fog. I believe this is due to the Spleen function. When patients reduced sugar, raw foods, and alcohol consumption many experienced marked relief from digestive trouble, an increase in energy, and clearer thinking. Better spleen function also translates to more blood to help nourish the muscles and sinews, which will improve symptoms of stiffness, as well as nourish the Heart and contribute to more restful sleep (Maciocia). Most patients will see the most benefit from also including herbs into their treatment. I have not included herbs in this overview, as I am currently only studying acupuncture—but would recommend someone take herbs in addition to an acupuncture treatment plan.
Conclusion
Research and case studies support the belief that fibromyalgia symptoms can be reduced in patients using a combination of acupuncture, herbs, exercise and patience. It is helpful to begin treatment as soon as possible, as it tends to progress into more serious and complex patterns as time goes on. The main organs involved are the Liver, Heart, Spleen and Kidneys and emotional stress is an important factor in the etiology and pathogenesis of Fibromyalgia. Education on lifestyle changes and stress management will help patients participate in their recovery and commit to a long-term collaborative treatment plan.
Sources
Cao, Hujuan; Liu, JianPing; Lewith, George T. Traditional Chinese Medicine for Treatment of Fibromyalgia: A Systematic Review of Randomized Controlled Trials. Alternative and Complementary Medicine. 2010, April; 16(4); 397-409
Cheng, Xinnong, and Liangyue Deng. Chinese Acupuncture and Moxibustion. Beijing: Foreign Language, 2010. Print.
Deare JC, Zheng Z. “Acupuncture for treating Fibromyalgia.” Compmed Health Institute, Southport, Queensland, Australia; RMIT University, Bundoora, Victoria, Australia, 3083. 2013 May 31;5 Retrieved August 20, 2013 from https://www.ncbi.nlm.nih.gov/pubmed/23728665
Maciocia, Giovanni. The Foundations of Chinese Medicine. Edinburgh: Elsevier Churchill Livingstone, 2005. Print. **I didn’t include page numbers for Maciocia or Cheng because this is general knowledge from these books and I didn’t quote specific pages.
Marcus, Alon. Fibromyalgia & OM. Chinese Herb Academy. Retrieved August 22,
2013 from https://www.chineseherbacademy.org/articles/Fibromyalgia_alon.shtml 1-7.
Mayo Clinic (2006, June 14). Acupuncture Relieves Symptoms Of Fibromyalgia, Mayo Clinic Study Finds. ScienceDaily. Retrieved August 22, 2013, from https://www.sciencedaily.com /releases/2006/06/060614000759.htm
Pfaffenberger, Angela H. TCM Diagnosis and Treatment of Fibromyalgia Syndrome. The Medical Acupuncture Web Page. Retrieved August 21st, 2013, from https://med-vetacupuncture.org/english/articles/fibro.html 1-5.
Wang, Douglas Yi. Acupuncture and Traditional Chinese Medical Approaches for Fibromyalgia. Acupuncture Today. March, 2005, Vol. 06, Issue 03. 1-3.
The contents of this site, including text, graphics, images, and other material are for informational purposes only. Nothing contained in this site is or should be considered or used as a substitute for professional medical or mental health advice, diagnosis, or treatment. Please schedule an appointment for personalized health advice.