Treating Systemic Lupus Erythematosus (SLE) with Acupuncture
Published on March 18, 2015 by Dr. Caitlin Gordon
What is it?
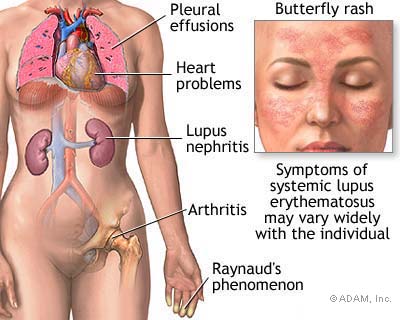 Systemic Lupus Erythematosus (SLE) is an autoimmune disorder marked by chronic inflammation in many organs and connective tissues of the body. Symptoms depend on the area of the body that is attacked and may change as the disorder progresses. Most common symptoms include:
Systemic Lupus Erythematosus (SLE) is an autoimmune disorder marked by chronic inflammation in many organs and connective tissues of the body. Symptoms depend on the area of the body that is attacked and may change as the disorder progresses. Most common symptoms include:
- joint pain and swelling
- fatigue
- hair loss
- mood changes
- Low-grade fever and
- increased sensitivity to sunlight.
- One of the hallmark signs is a butterfly-shaped rash across the bridge of the nose but this does not appear in all cases (Zhang).
Western medicine diagnoses this condition by using a combination of tests including an antinuclear antibody (ANA) blood test (St. Juste). In 95% of cases, this test will come back positive. Other tests are necessary to pinpoint the problem. Tests for anemia, skin biopsies, urinalysis and other examinations may be ordered. Women are more often affected than men.
What causes it?
Western medicine does not know the cause of SLE but believes it to be a combination of genetic factors and autoimmune dysfunction. Certain medications may also cause a patient to develop SLE. While there is no cure, there are a variety of anti-inflammatory and immunosuppressant drugs, which may be prescribed to manage symptoms. As the disease progresses it may affect critical body systems like the heart and kidneys. Renal failure is the major cause of death. Alternative treatments like acupuncture play an important role in managing symptoms, as the medications available often have very unpleasant side effects.
Lupus and Acupuncture

At its core lupus is an imbalance of yin and yang in the body according to Traditional Chinese Medicine (TCM). There is either too much Yang creating fire and toxic heat in the body, or not enough Yin, resulting in Yin-deficient internal heat. There may also be a combination of symptoms due to both excess and deficient heat. Other aspects of the disorder, in particular, painful swollen joints fall under a diagnosis of Heat Bi Syndrome in TCM.
Toxic Heat/Fire
Symptoms of Fire, and in chronic cases, toxic heat, include butterfly rash, thirst, constipation, red complexion, fever and dark scanty urine. The tongue will present with a red body and greasy yellow coat. Pulse will be rapid and full or taut (Zhang). Fire can be an excess of Yang in the body. This explains why SLE symptoms are often worse in young people. Flare-ups have a tendency to be more intense as the “Yang energy among young people is more intense than the old (Stone, 2).” When there isn’t enough Yin to cool the fire of the Yang, it becomes excessive. There is already a relative imbalance in favor of more Yang energy in the young.
Giovanni Maciocia discusses how toxic heat or Fire can cause the symptoms listed above. First, Fire is a Yang pathogenic factor and it rises. It can agitate the mind and cause irritability and mood changes, which are common symptoms of SLE (Maciocia, 702). Fire is very drying and causes constipation and dark scanty urine. Because it is so drying, Fire often damages Blood and Yin. This is responsible for the majority of the symptoms experienced by the SLE patient. This explains why the disease may begin with an etiology of Fire but transition into a Yin-deficient internal heat (Cheng). Blood and Yin deficiency especially affect the Liver and Kidneys and are discussed in more detail in the next section.
Fire will affect different organ systems differently. For example, if the patient experiences jaundice (yang jaundice), abdominal distention, anorexia, or nosebleeds, this is categorized as an “impairment of the liver due to heat and treatment should be aimed at soothing the liver, regulating the circulation of qi and promoting blood circulation to remove stasis (Zhang).”
Finally, Fire causes ulcers and swelling. This explains the red swollen joint pain that is further classified as Heat Bi in some SLE sufferers. Because heat rises, Fire may cause ulcers or chancre sores in the mouth. This may be full or empty-heat in nature, often relating to a deficiency of Yin in the Stomach. If it is a Stomach-Yin Deficiency, “the patient will feel heartburn most pronounced when the stomach is empty (Stone).” If it is excess heat, the heartburn or stomach pain will be more pronounced on a full stomach. Treatment would be focused on clearing toxic heat, tonifying Yin, cooling blood and fortifying the internal organs.
Yin Deficient Internal Heat
Symptoms of Yin Deficiency with Internal Heat include night sweats, insomnia, low-grade fever, fatigue, joint pain and hair loss. The tongue will be red with either a thin yellowish fur or peeled. Pulse will be thready and rapid (Zhang). Maciocia states that the “deficiency of Yin involves the excessive consumption of Body Fluids, the Yin substances of each organ, the Essence, and Blood (Maciocia, 400).” Liver and Kidneys are particularly affected by a Blood and Yin deficiency. Corresponding symptoms include Alopecia and Photosensitivity.
Photosensitivity or Photophobia is an aversion to bright lights or even normal light that appears painfully bright to sufferers. In TCM, Liver blood is in charge of “nourishing and lubricating the eyes with tears (Stone, 2).” When Liver-Yin is deficient the eyes become dry and sensitive. Blurriness and vertigo, as well as dizziness, are other SLE symptoms that may accompany a diagnosis of Liver-Yin Deficiency in TCM.
Alopecia is the thinning of hair. It is associated with Yin deficiency because in order for hair to be healthy there needs to be an adequate amount of Blood and Fluids. Liver blood nourishes the hair. Also, the Kidneys are associated with the hair on the head, so Kidney-Yin deficiency may manifest as Alopecia in patients with SLE (Maciocia).
A deficiency of Liver blood may also cause the common joint pain experienced by those with SLE. Liver blood nourishes and lubricates the tendons, and without adequate blood, there will be arthritic symptoms. Joint pain is also related to a lack of Jin-Ye, which is common in Yin deficiency and with excess heat as it dries the fluids (Maciocia). Treatment would be focused on replenishing the Yin and clearing empty heat to calm the body’s inflammatory response and relieve symptoms.
Heat Bi Syndrome
Heat bi syndrome is characterized by redness, pain, and swelling. In the case of SLE it is in the joints and may move from joint to joint as is typical in Wind Bi syndrome or be localized to some areas of the body like knees or wrists most commonly. According to Cheng Xinnong’s Chinese Acupuncture and Moxibustion (CAM), one of the causes of bi syndrome is “body constitution with exuberant yang qi and accumulated heat, invasion of pathogenic wind, cold and damp (Cheng).” Fire may also generate wind, according to Maciocia, further explaining the concurrence of symptoms associated with SLE. Treatment would focus on dispelling the wind, the damp and clearing heat.
Recent Research
A study in 2008 investigated the safety and efficacy of treating SLE with acupuncture. As summarized in the abstract, the study randomly selected 24 individuals with SLE to receive ten sessions of acupuncture, minimal needling, or standard care. Out of these, 22 completed the study and “40% of the patients in the acupuncture and minimal needling groups showed an improvement greater than 30 percent using a standard measure of pain. There was no improvement in pain in the standard care group (Greco).” The other studies related to lupus have been based on specific symptom relief or related autoimmune diseases such as Rheumatoid Arthritis and Scleroderma. Unfortunately, there have been very limited published studies specific to SLE and TCM treatment.
Case Studies
I read through a number of case studies and in each instance, the onset of lupus symptoms was associated with a trauma or stressful life event. This coincides with the etiology theories of TCM that say the body is more susceptible to pathogenic influences as well as Yin/Yang imbalances when under stress. Chronic long-term stress also creates Yin deficiency, which matches with the symptoms most SLE sufferers experience. Another pattern was a history of antibiotic use and disorders of the Chong and Ren meridians. Antibiotic use can destroy the healthy balance of intestinal flora and lead to poor absorption of nutrients, impaired immune function, and Yin deficiency. Disorders of the Chong and Ren, often caused by long-term use of hormonal birth control can lead to stagnation in the Lower Jiao which impairs the smooth flow of qi throughout the body, in particular, the flow of liver qi leading to liver blood deficiency and liver heat (Maciocia).
Conclusion
 Acupuncture treatments focused on addressing a diagnosis of either Fire or Yin Deficient Internal Heat, along with symptom-specific diagnosis and differentiation like Heat Bi for those suffering from hot swollen joint pain would provide relief for patients with SLE. There may not be a cure, but reducing the body’s inflammatory response and relieving pain and swelling would be a great benefit. Nourishing yin and building blood would help relieve symptoms like insomnia, night sweats, alopecia, photosensitivity, mood swings, and fatigue.
Acupuncture treatments focused on addressing a diagnosis of either Fire or Yin Deficient Internal Heat, along with symptom-specific diagnosis and differentiation like Heat Bi for those suffering from hot swollen joint pain would provide relief for patients with SLE. There may not be a cure, but reducing the body’s inflammatory response and relieving pain and swelling would be a great benefit. Nourishing yin and building blood would help relieve symptoms like insomnia, night sweats, alopecia, photosensitivity, mood swings, and fatigue.
In many chronic diseases, it is important to tonify the immune system. However, in cases of autoimmune disorders, characterized by the body attacking itself, this may actually aggravate symptoms. It is necessary to tonify but without fueling the heat and inflammation response. By balancing the body’s Yin and Yang and fortifying weak organ systems we can attempt to activate the body’s own healing system to bring the immune response back into equilibrium. Autoimmune disorders are often more successfully treated by alternative modalities like Traditional Chinese Medicine since they focus on bringing the body back into harmony naturally without the need to suppress the immune system with pharmaceuticals.
⇒Schedule an appointment or a free consultation to discuss acupuncture treatment.
Sources:
Cheng, Xinnong, and Liangyue Deng. Chinese Acupuncture and Moxibustion. Beijing: Foreign Language, 2010. Print.
Greco, C., A. Kao, K. Maksimowicz-McKinnon, R. Glick, M. Houze, S. Sereika, J. Balk, and S. Manzi. “Acupuncture for Systemic Lupus Erythematosus: A Pilot RCT Feasibility and Safety Study.” Lupus 17.12 (2008): 1108-116. Print.
Maciocia, Giovanni. The Foundations of Chinese Medicine. Edinburgh: Elsevier Churchill Livingstone, 2005. Print.
St. Juste Jr., Carlo, L.Ac. “Systemic Lupus Erythematosus at a Glance.” Mma Acupuncture. N.p., 13 Feb. 2012. Web. 11 Dec. 2012.
Stone, Al, L.Ac. “Lupus and Traditional Chinese Medicine.” VitalityLink. Vitality Link, 19 Dec. 2011. Web. 10 Dec. 2012.
Zhang, Engin Dr. A Practical English-Chinese Library of Traditional Chinese Medicine. London: Middlesex University Archway Campus, 2009. Print.
The contents of this site, including text, graphics, images, and other material are for informational purposes only. Nothing contained in this site is or should be considered or used as a substitute for professional medical or mental health advice, diagnosis, or treatment. Please schedule an appointment for personalized health advice.