Treating Overactive Bladder with Acupuncture
Published on November 14, 2014 by Dr. Caitlin Gordon
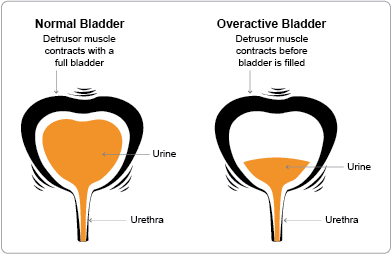
Overactive bladder affects as many as 1 in 6 adults in the United States and becomes more common with age. The following signs and symptoms mark the condition:
- Urgency: You feel a sudden urge to urinate that is difficult to control.
- Frequency: You urinate 8 or more times in 24 hours.
- Nocturia: You awaken two or more times in the night to urinate.
- Urge Incontinence: You experience an involuntary loss of urine immediately following the need to urinate.
There may also be dribbling, incontinence with sneezing or laughing, or stress incontinence but these alone do not qualify as overactive bladder syndrome. The filling and emptying of the bladder directly involve the kidney system and a complex interplay of nerve signals and muscle activity in the bladder, urethra, and brain. A problem in any of these systems can contribute to overactive bladder symptoms.
 Urologists have been treating overactive bladder symptoms with acupuncture for years though most people are unaware as they call it something else. The term commonly used by urologists is Percutaneous posterior Tibial Nerve Stimulation (PTNS) or “Stoller afferent nerve stimulation,” which is one of the neuromodulation techniques. PTNS targets the mixed nerve just above the ankle (containing both motor and sensory nerve fibers) using a 36 gauge acupuncture needle attached to an electric stimulator. The tibial nerve then carries the electrical signals to the sacral spine. Typically, this procedure lasts 30 minutes and is administered weekly for 3 months. Interestingly, the point chosen by urologists for PTNS is the acupuncture point SP 6. The electrical stimulation is identical, to the electro-acupuncture technique commonly used by Traditional Chinese Medicine (TCM) practitioners.
Urologists have been treating overactive bladder symptoms with acupuncture for years though most people are unaware as they call it something else. The term commonly used by urologists is Percutaneous posterior Tibial Nerve Stimulation (PTNS) or “Stoller afferent nerve stimulation,” which is one of the neuromodulation techniques. PTNS targets the mixed nerve just above the ankle (containing both motor and sensory nerve fibers) using a 36 gauge acupuncture needle attached to an electric stimulator. The tibial nerve then carries the electrical signals to the sacral spine. Typically, this procedure lasts 30 minutes and is administered weekly for 3 months. Interestingly, the point chosen by urologists for PTNS is the acupuncture point SP 6. The electrical stimulation is identical, to the electro-acupuncture technique commonly used by Traditional Chinese Medicine (TCM) practitioners.
A single PTNS treatment with an MD or urologist can cost anywhere from 300-600$. Doing the necessary series of 12-15 treatments will cost you thousands. Save money (over 50% less expensive) and get the added benefit of a full acupuncture treatment (relaxation, stress relief, better sleep, more energy!) by seeing a licensed acupuncturist familiar with this technique. If you’re in Colorado, you can schedule online to come see me for PTNS..
Several studies from 1982-1999 showed significant improvement in treating overactive bladder with acupuncture using the PTNS procedure—essentially electro-acupuncture at SP 6. Results were noted even after a single treatment. Despite all the promising data, this was not a common treatment among urologists until February 2000 when an FDA approved electrostimulation unit became commercially available. A growing number of urology clinics have been using the procedure ever since. Urology specialists have recommended that PTNS is “useful for treating refractory urinary urge incontinence and should at least be considered as a therapeutic alternative before resorting to an aggressive surgery (Van Balken).” PTNS is contraindicated for patients wearing pacemakers or defibrillators. It is also not recommended for patients with coagulopathy (a tendency toward bleeding) or neuropathy, or for pregnant women.
Traditional Chinese Medicine and Overactive Bladder
 In TCM, we often see overactive bladder as being a problem with “kidney qi”. There are various ways to strengthen the kidneys through acupuncture, herbal medicine, and diet, as well as physical muscle strengthening and retraining of the neural pathways. One of the more popular studies showing positive effects treating overactive bladder with acupuncture is as follows:
In TCM, we often see overactive bladder as being a problem with “kidney qi”. There are various ways to strengthen the kidneys through acupuncture, herbal medicine, and diet, as well as physical muscle strengthening and retraining of the neural pathways. One of the more popular studies showing positive effects treating overactive bladder with acupuncture is as follows:
A study by Emmons SL and Otto L compares acupuncture treatment for overactive bladder with placebo acupuncture treatment. The trial, called “Acupuncture for overactive bladder: a randomized controlled trial”, is dated 2005 and performed at the Department of Obstetrics and Gynecology at the Oregon Health and Science University in Portland, OR. It looked at 85 women who were randomly assigned to receive an acupuncture treatment designed to improve their bladder symptoms or a placebo treatment designed to promote relaxation. The acupuncture treatment for bladder issues utilized bilateral insertion at 4 acupuncture points on each side of the body. Needles were placed and rotated clockwise until the patient reported a sensation of warmth or tightening, then were retained without further stimulation for 20 minutes. The placebo acupuncture treatment designed for relaxation used 4 different bilateral points. Both groups received 4 weekly acupuncture treatments and tracked their urination with cystometric testing, a urinary distress inventory, a 3-day voiding diary, and an incontinence impact questionnaire. The study measured the number of incontinent episodes as well as voiding frequency and urgency, distress, maximum voided volume and cystometric bladder capacity. There were 74 women who completed the full study. Both women in the treatment and placebo groups had decreases in the number of incontinent episodes. There was a 59% reduction for the acupuncture treatment group and 40% for the placebo group. Women receiving acupuncture treatment for urinary issues had a 14% reduction in frequency, and 13% increase in maximum voided volume and cystometric capacity. The study concluded that the 4 weekly bladder specific treatments were significantly more effective than the placebo relaxation treatment.
⇒If you’d like to try treating your overactive bladder with acupuncture, schedule today.
Sources
- Emmons SL, Otto L: Acupuncture for overactive bladder: A randomized controlled trial. Obstetrics and Gynecology 2005, 106(1):138-143. 15.
- Stoller ML: Afferent nerve stimulation for pelvic floor dysfunction. European Urology 1999, 35 (Suppl 2):1-196.
- Van Balken MR, Vandoninck V, Gisolf KW, Vergunst H, Kiemeney LA, Debruyne FM, Bemelmans BL: Posterior tibial nerve stimulation as neuromodulative treatment of lower urinary tract dysfunction. The Journal of Urology 2001, 166(3):914-918.
- Bergstrom K, Carlsson CP, Lindholm C, Widengren R: Improvement of urge- and mixed-type incontinence after acupuncture treatment among elderly women – A pilot study. Journal of the Autonomic Nervous System 2000, 79(2-3):173-180.
- Van Balken MR, Vergunst H, Bemelmans BL: Prognostic factors for successful percutaneous tibial nerve stimulation. European Urology 2006, 49(2):360-365.
The contents of this site, including text, graphics, images, and other material are for informational purposes only. Nothing contained in this site is or should be considered or used as a substitute for professional medical or mental health advice, diagnosis, or treatment. Please schedule an appointment for personalized health advice.